When I lost my period at age 14, my doctor’s solution was simple: birth control pills.
No questions about my diet. No questions about my exercise habits.
No investigation into why a healthy teenager would suddenly stop menstruating.
For the next 13 years, I took those pills thinking I was having normal periods each month.
What I didn’t realize was that the bleeding I experienced wasn’t a real period at all—just withdrawal bleeding from synthetic hormones.
It wasn’t until I finally stopped birth control years later that I discovered the truth: my period was still missing, and I had a condition called hypothalamic amenorrhea.
What Is Hypothalamic Amenorrhea?
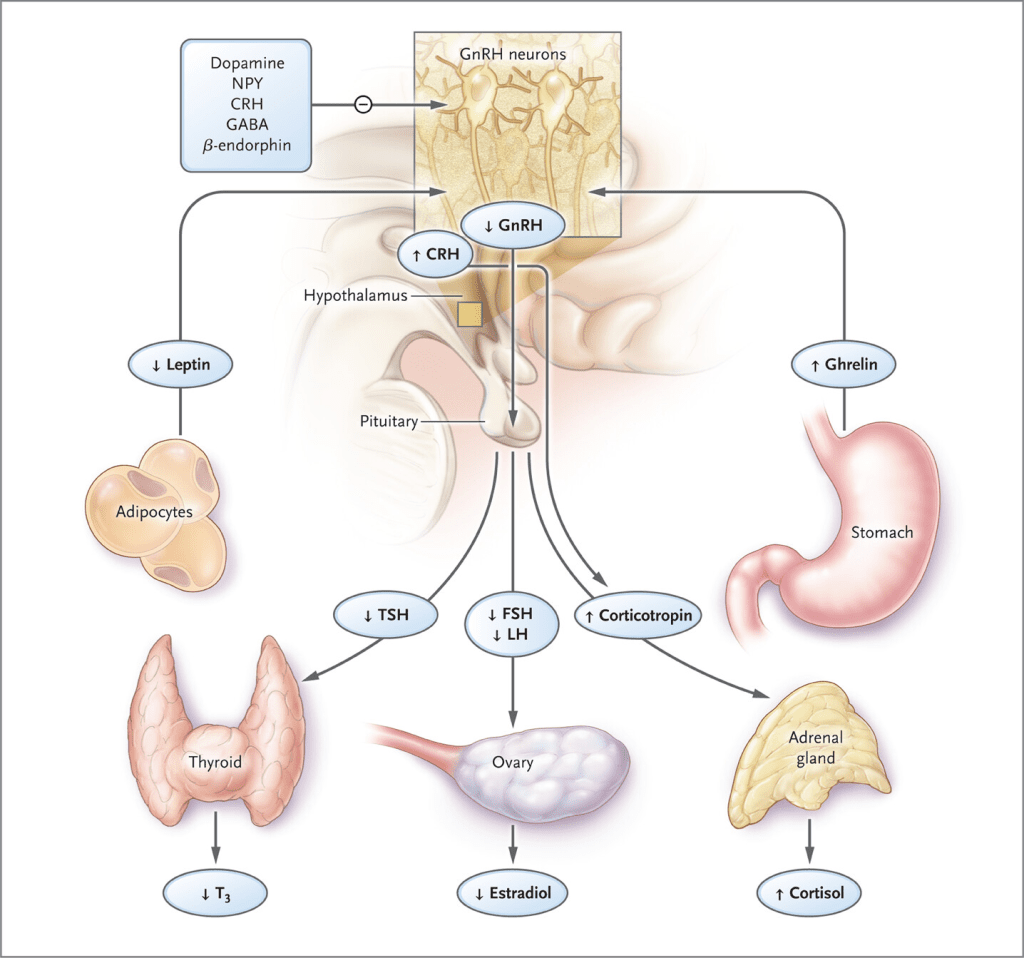
Hypothalamic amenorrhea (HA) is when your brain’s command center—the hypothalamus—stops sending hormones needed for ovulation and menstruation.
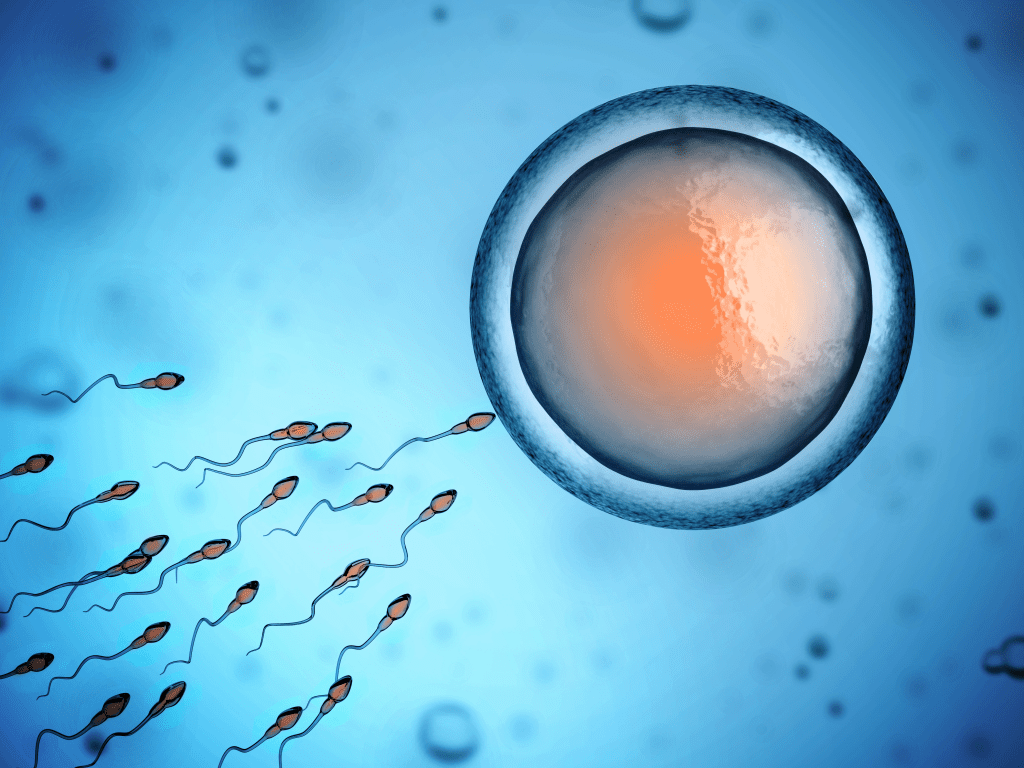
The hypothalamus releases a hormone called gonadotropin-releasing hormone (GnRH), which then stimulates the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH), essential for sperm production, ovulation, and estrogen and progesterone production.
Without these hormones, your ovaries can’t produce estrogen and progesterone properly, and your menstrual cycle shuts down.
Your body is smart. When it detects threats like low nutrition, too much exercise, high levels of stress, or a combination of these factors—it essentially says:
“I don’t have enough resources for reproduction. Let’s focus on survival instead.”
Why HA Is Commonly Misdiagnosed or Missed
I was misdiagnosed multiple times (by some of the best doctors in the field). I went on to discover that this happens more often than you might think!
Here are 2 major reasons why:
Mistaken for PCOS:
Many women with HA are incorrectly diagnosed with polycystic ovarian syndrome (PCOS). This is because both can cause irregular or missing periods.
Plus, PCOS has become the overarching, go-to diagnosis for anyone who has missing and irregular periods.
Multiple doctors diagnosed me with PCOS despite having none of the typical symptoms like elevated androgens, excess hair growth, or acne.
Masked by birth control:
Hormonal contraceptives create artificial cycles that hide the underlying problem.
This is what happened to me for 13 years—I appeared to have normal periods on birth control, but my natural cycle was completely suppressed.
3 Common Causes of Hypothalamic Amenorrhea
1. Energy Deficiency

The most fundamental cause of HA is not providing your body with enough calories to support both basic functions and reproduction.
This doesn’t necessarily mean you’re starving yourself—you might be eating what seems like “enough” but not enough for your individual needs, especially if you’re active.
Exercise is good. Being mindful of your nutrition and calories is good. But the notion that you have to spend all your time working out and eat like a rabbit has ruined many women’s fertility.
In my case, I was running daily while restricting calories—a perfect storm for shutting down my reproductive system.
2. Psychological Stress

Your body doesn’t distinguish between different types of stress—physical or psychological, they all trigger similar hormonal responses. Chronic stress elevates cortisol levels, which directly inhibits GnRH production in the hypothalamus.
3. Rapid Weight Loss or Low Body Fat

Your body needs a minimum amount of fat to maintain proper hormone production. Adipose tissue isn’t just for energy storage—it actively participates in producing and regulating reproductive hormones.
The sweet spot for fertility is between 22-32% body fat for women. Every woman is different so the optimal body fat that a woman needs to have healthy cycles will vary. But in general, anything lower than 22% is a sign that the body does not have enough fat to make reproductive hormones.
How I Healed My Hypothalamic Amenorrhea
After seeing multiple doctors who just wanted to put me back on birth control, I finally found a functional medicine specialist who recognized what was happening.
Together, we created a recovery plan that finally addressed the root causes of my condition (without any drugs or unnecessary procedures). Here’s a quick overview of everything we did:
1. Increasing Caloric Intake
The single most important factor in my recovery was eating more—significantly more. I increased my daily intake by approximately 500-700 calories, focusing on:
- Healthy fats: Butter, full-fat dairy, nuts, and seeds became daily staples
- Quality protein: Red meat, eggs, fatty fish, and other animal proteins at every meal
- Carbohydrates: Lots of fruits and complex carbs to give my cells energy
Moreover, I made sure to eat 3 meals a day and 1-2 snacks minimum.
This wasn’t just about gaining weight (though I did gain about 15 pounds in the process).
It was about sending my body consistent signals that resources were abundant and it was safe to resume reproductive functions.
2. Transforming My Exercise Routine
I completely reimagined my relationship with movement:
- Reduced high-intensity cardio sessions
- Avoided exercising more than once a day
- Limited exercise to 1 hour per session, max
- Focused on strength training and walking
- Added restorative activities like yoga and stretching
The hardest part wasn’t changing the workouts themselves but changing my mindset.
I had to stop viewing exercise as a calorie-burning necessity and start seeing it as a way to strengthen my body and be more in-tune with it.
3. Stress Management Practices
I implemented daily stress reduction techniques:
- Morning walks with my dog
- Regular acupuncture sessions
- Setting better boundaries in my work and personal life
- Breathing techniques
- Prioritizing 7-8 hours of quality sleep
4. Targeted Supplementation
The last piece of the puzzle is supplements.
Supplements are only useful once you have the foundations mentioned above covered.
Supplements should also be personalised to your body and your needs.
These supplements helped me personally:
- Magnesium: Research shows it helps regulate the HPA axis (hypothalamic-pituitary-adrenal) that controls stress responses
- Vitamin D: Improves hormonal production and regulation
- Ashwagandha & Maca: Used temporarily to reduce stress and support hormonal balance
- Methylated B-complex: To increase cellular energy production and support overall metabolism
How Long Does Recovery Take?
For me, it took approximately 6 months from when I started actively working with my functional medicine doctor until my first natural period returned.
That moment—waking up to finally see blood—was indescribable. The relief and validation that my body could heal after 16 years of dysfunction felt like a miracle.
And within five months of getting my period back, I was able to conceive naturally.
It usually takes 2-6 months to get your periods back. But it can take longer or shorter based on :
- Duration of amenorrhea (longer cases typically take more time to resolve)
- Severity of energy deficiency
- Individual hormonal baselines
- Consistency in implementing recovery strategies
7 Signs You Might Have Hypothalamic Amenorrhea
If you’re experiencing any of these symptoms (especially in combination) consider talking to a healthcare provider about HA:
- Missed periods for 3+ months (not due to pregnancy, breastfeeding, or menopause)
- Low energy and persistent fatigue despite adequate sleep
- Constantly feeling cold, especially in your extremities (a sign of lowered metabolism)
- Low libido and vaginal dryness from reduced estrogen
- Sleep disturbances despite feeling tired
- Frequent injuries or stress fractures
- History of restrictive eating and/or intensive exercise regimens
Getting Proper Diagnosis
I would hate for you to get misdiagnosed and keep moving from doctor to doctor, desperate for a solution. Make sure you’ve done all of these tests before accepting any diagnosis:
- Complete hormone panel: Including estradiol, LH, FSH, prolactin, and thyroid hormones
- DEXA scan: To assess bone mineral density if periods have been absent for over a year
- Thorough medical history: Including detailed discussion of diet, exercise, and stress levels
Be careful because many conventional doctors are quick to prescribe birth control rather than addressing root causes. At Ferta, we take the functional, integrative approach.
Click here to book a free consultation with our fertility specialist and let’s see if you’re a good fit for us!
The Bottom Line on Hypothalamic Amenorrhea
Hypothalamic amenorrhea is a warning sign that your body is under stress—whether from inadequate nutrition, excessive exercise, psychological pressure, or a combination of these factors.
It’s not something to ignore or mask with hormonal contraceptives.
But HA is 99% reversible. Your body has an incredible capacity to heal when given the right environment and resources. As someone who recovered after 16 years without a natural period, I am proof that healing is possible (even in long-standing cases).
If you’re struggling with missing periods, know that you’re not alone.
With the right approach—one that addresses the root causes rather than just the symptoms—you can restore your hormonal health and get your periods back.
Have you experienced hypothalamic amenorrhea or are you currently dealing with missing periods? Share your experience in the comments below.
At Ferta, we specialize in helping women restore their natural hormonal balance and fertility. If you’re struggling with hypothalamic amenorrhea or other hormonal issues, our team of experts can create a personalized protocol to support your body’s healing process. Book a consultation to learn more.