If you’ve found yourself Googling “how long does Metformin diarrhea last” while sitting on the toilet with a heating pad on your ovaries and tears in your eyes.
Hi! We see you.
Let’s talk about it. The science. The survival tips.
And most importantly, the hope they (Big Pharma) don’t want you to know about.

When PCOS Meets Metformin (and Your Gut Panics)
Polycystic Ovary Syndrome affects about 1 in 10 women globally, and it’s not just about missed periods or hormonal acne.
It’s a whole-body metabolic condition, and one that modern medicine still largely treats with a shrug and a script for Metformin.
Metformin’s role? It helps improve insulin sensitivity, lower circulating insulin levels, and often supports more regular ovulation in people with PCOS.
But here’s the catch:
Metformin vs. Your Gut = A Battle Your Bathroom Wasn’t Prepared For
The side effects can feel like an intestinal apocalypse: gas, bloating, cramping, and es!
Those infamous surprise bathroom emergencies.
If you ever had to excuse yourself from a job interview because of a Metformin moment, let us assure you.
You are not alone.

The Hidden Science: What’s REALLY Happening Inside Your Body
When your doctor prescribes Metformin for PCOS, they rarely explain the complex cascade of events about to unfold in your digestive system.
Here’s what they don’t tell you:
Phase 1: The Initial Contact (Days 1-7)
The moment Metformin enters your system, it begins altering the transportation of glucose across intestinal cell membranes.
Specifically, it inhibits the sodium-glucose cotransporter-1 (SGLT1), which is responsible for glucose absorption in your intestines.
This immediate change causes unabsorbed glucose to remain in your intestinal lumen, creating an osmotic effect.
Basically, water gets pulled into your intestines instead of being absorbed by your body.
The result? Looser stools and more frequent trips to the bathroom.
Simultaneously, Metformin begins activating AMP-activated protein kinase (AMPK) in your liver, which starts reducing glucose production.
While great for insulin resistance, this rapid metabolic shift can trigger nausea and digestive discomfort as your body struggles to adapt.
Phase 2: The Microbiome Revolution They Won’t Discuss (Weeks 1-4)
By week two, Metformin begins dramatically reshaping your gut microbiome.
Research published shows specific changes:
- Fewer Intestinibacter hanging around
These guys are part of your gut’s peacekeeping squad, so when their numbers drop, things can get a little rowdy. - A big boost in Akkermansia muciniphila (up to 4x!)
This overachiever munches on your gut lining’s mucus (sounds gross, actually great) and helps keep your metabolism and gut barrier in check. - More Butyrivibrio in the mix
They’re the butyrate producers, aka the gut’s version of anti-inflammatory superfood, keeping your colon calm and happy.
These bacterial shifts aren’t random side effects.
They’re actually part of how Metformin works.
Akkermansia muciniphila helps regulate glucose metabolism and reduces inflammation.
However, this microbiome transformation comes at a cost.
As these bacterial populations shift, they produce different metabolites and short-chain fatty acids than your body is accustomed to.
This change in gut chemistry can trigger:
- Increased gas production (especially hydrogen and methane)
- Alterations in intestinal pH
- Changes in the rate of peristalsis (the wave-like contractions that move food through your digestive system)
During this phase, many women experience the WORST digestive symptoms as their gut ecosystem is essentially being reconstructed without their consent!
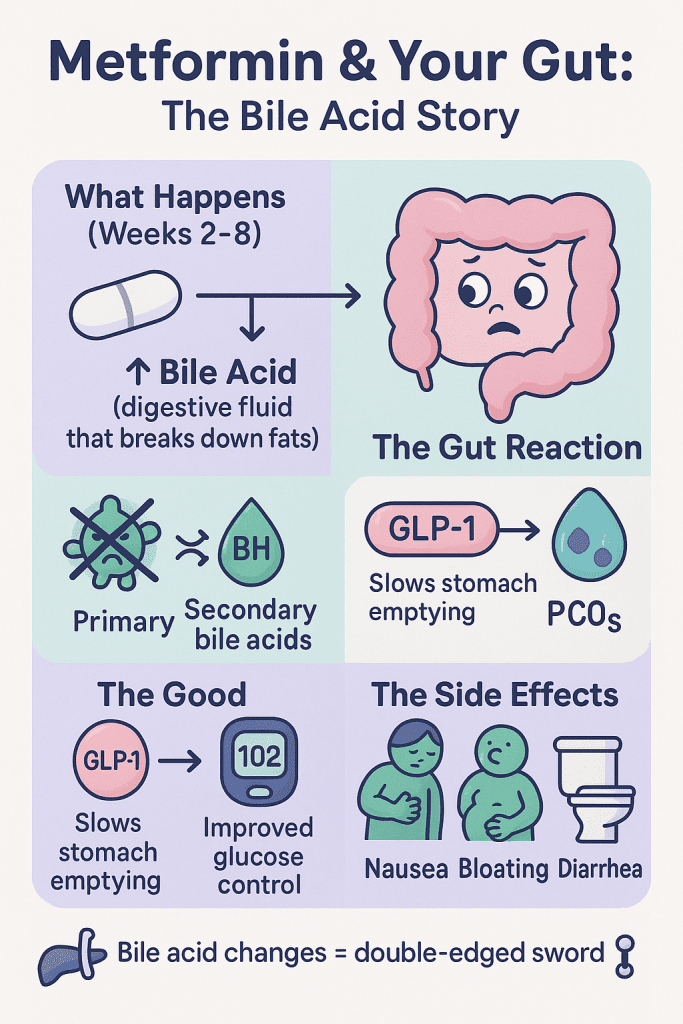
Phase 3: Bile Acid Disruption (Weeks 2-8)
What most doctors don’t explain is that Metformin also increases the amount of bile acid. It’s a digestive fluid that helps break down fats in your intestines.
A study in the Journal of Endocrinology found that Metformin alters the ratio of primary to secondary bile acids by inhibiting the bile salt hydrolase activity of certain gut bacteria.(https://pmc.ncbi.nlm.nih.gov/articles/PMC6328020/)
This change in bile acid composition has two major effects:
- It enhances the medication’s blood-glucose-lowering effects (good for PCOS)
- It stimulates the secretion of glucagon-like peptide-1 (GLP-1), which slows gastric emptying
The slowed stomach emptying can contribute to nausea and bloating, while the altered bile acid composition often triggers diarrhea by increasing intestinal motility and fluid secretion.
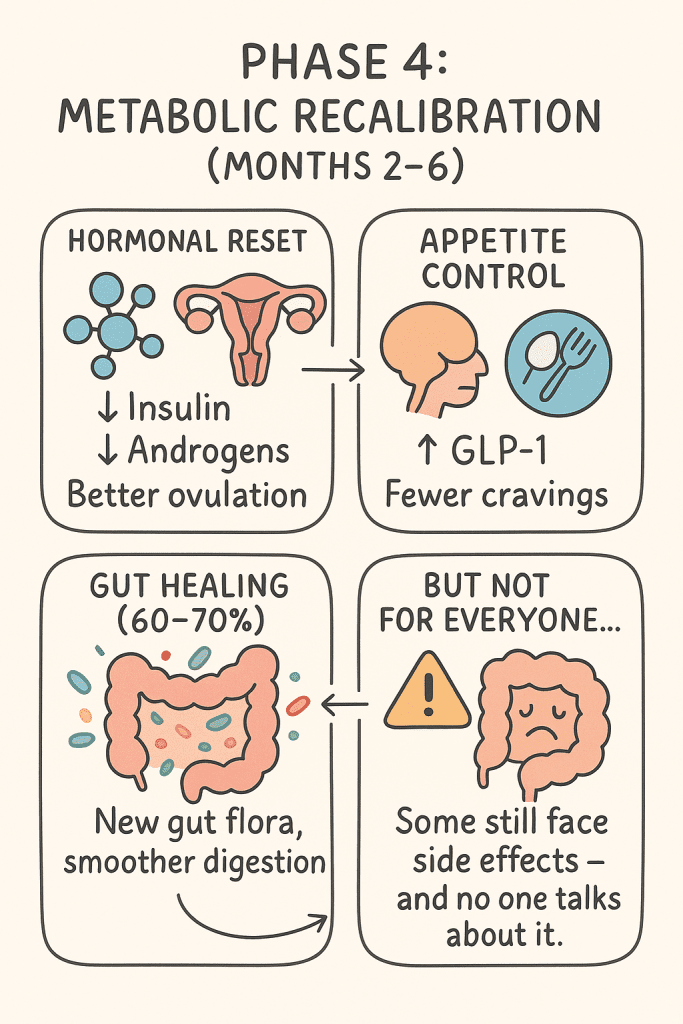
Phase 4: Metabolic Recalibration (Months 2-6)
If you can make it through the first few months, your body begins adapting to these changes. The improved insulin sensitivity starts to positively affect your hormonal balance:
- Insulin levels decrease, which reduces the stimulation of androgen production in your ovaries
- Lower androgen levels allow for more regular follicle development
- GLP-1 increases, which improves satiety signals and often reduces cravings
For about 60-70% of women, digestive symptoms begin to improve during this phase as the gut adapts to the new bacterial ecosystem and bile acid profile.
But for others, the side effects persist.
That’s the dirty truth they don’t warn you about when handing over that prescription.

Why Traditional Approaches Fall Short
The conventional medical approach to PCOS often overlooks the complex interconnection between insulin resistance, gut health, and hormonal balance.
When you’re prescribed Metformin without addressing these underlying factors, you’re essentially getting a partial solution with uncomfortable side effects.
What’s really happening in your body with PCOS goes beyond just elevated androgens or irregular periods.
It’s a whole-body metabolic condition involving:
- Insulin resistance in multiple tissues (not just your liver)
- Systemic low-grade inflammation affecting hormone receptors
- Gut dysbiosis that impacts everything from nutrient absorption to hormone metabolism
- HPA axis disruption (the communication pathway between your brain and hormonal glands)
Metformin addresses primarily the insulin resistance component.
Important, but just one piece of the puzzle they’re not showing you.
The Ferta Approach: A Body-First Solution They Don’t Want You To Know About
At Ferta, we’ve developed a comprehensive system that works with your body’s natural processes instead of forcing change through pharmaceutical intervention.
Here’s exactly how our approach works, step by step:
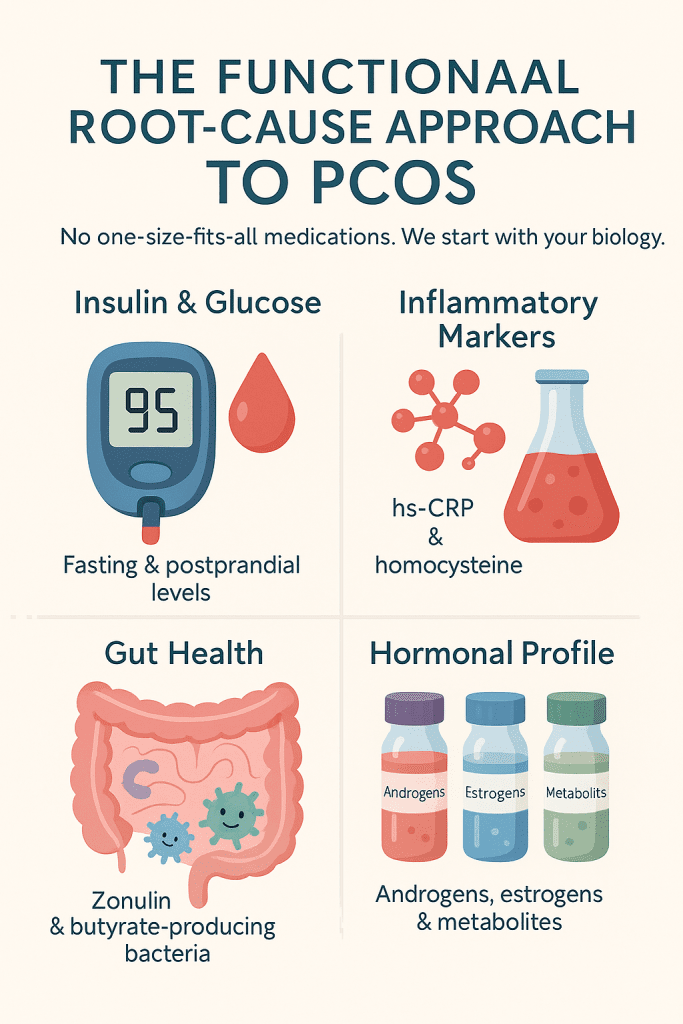
Step 1: Comprehensive Metabolic Assessment (Week 1)
Unlike conventional PCOS treatment that jumps straight to medication, we begin with a detailed analysis of your:
- Fasting and postprandial insulin and glucose levels
- Inflammatory markers including hs-CRP and homocysteine
- Gut health indicators including zonulin and butyrate-producing bacteria
- Complete hormonal profile including androgens, estrogens, and their metabolites
This gives us a precise map of what’s happening in your unique body, rather than treating you with a one-size-fits-all approach that pharmaceutical companies profit from.
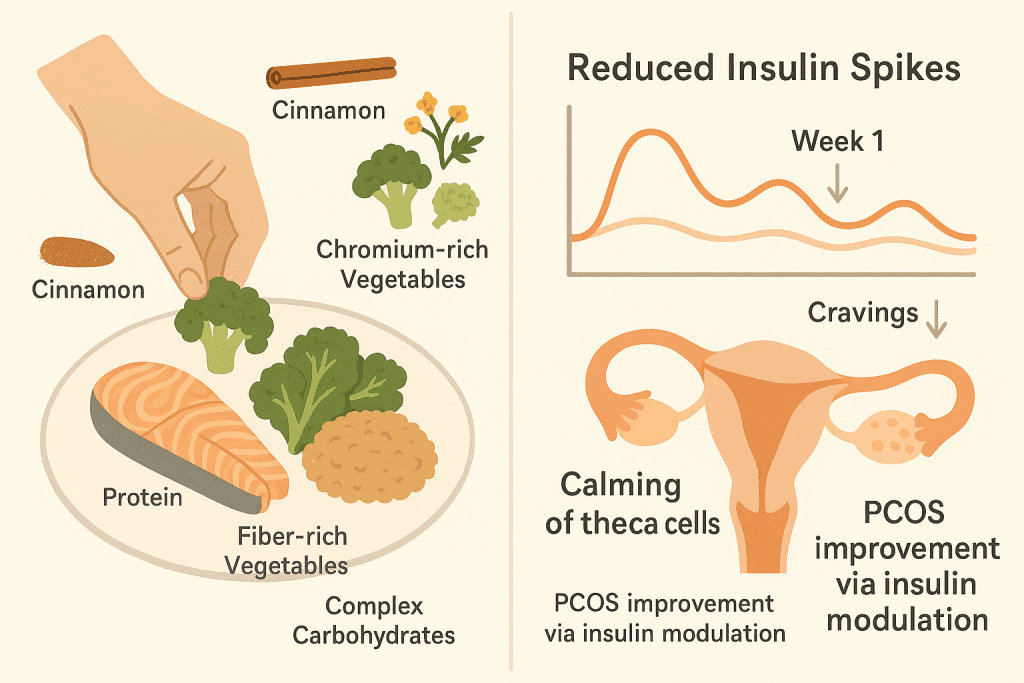
Step 2: Stabilizing Blood Sugar Through Nutritional Intelligence (Weeks 1-4)
Rather than forcing insulin sensitivity through medication, we teach your body how to naturally regulate blood sugar through precisely timed nutrition.
Our clients begin with:
- Structuring meals with protein first, followed by fiber-rich vegetables, and complex carbohydrates last
- Implementing a 12-hour gentle overnight fast to improve insulin sensitivity
- Adding specific blood-sugar stabilizing foods like cinnamon, berberine-containing herbs, and chromium-rich vegetables
Within days, many women notice reduced cravings and more stable energy. Within weeks, fasting insulin levels begin to normalize.
This happens without the digestive distress of Metformin because we’re working WITH your body’s natural processes, not against them.
The science: This approach reduces both the amplitude and frequency of insulin spikes, which immediately begins calming the ovarian theca cells that produce excess androgens in PCOS.
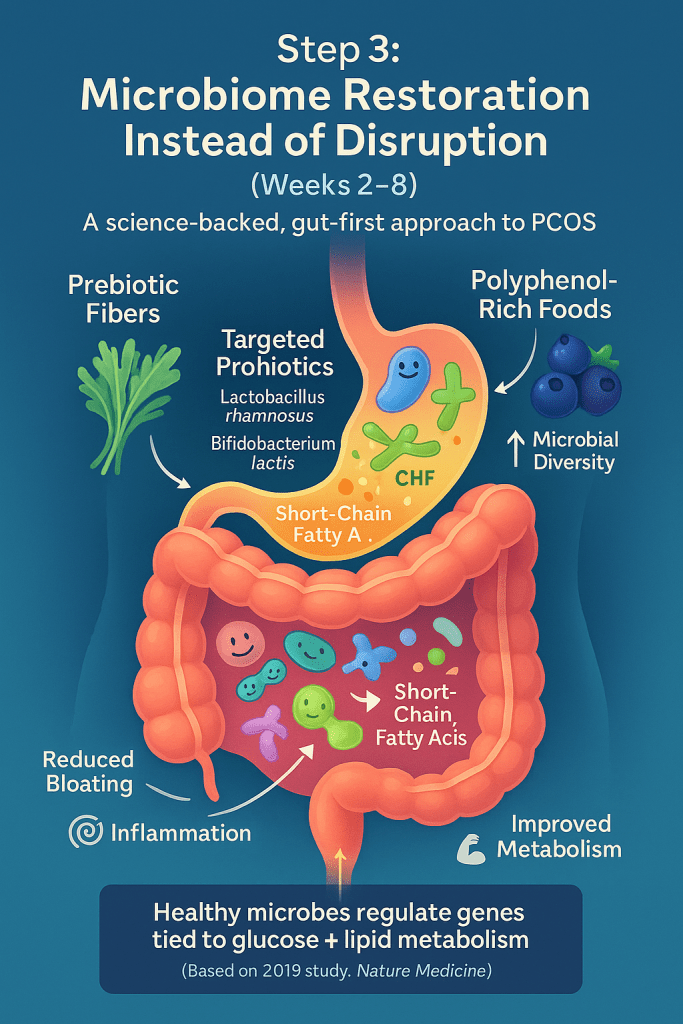
Step 3: Microbiome Restoration Instead of Disruption (Weeks 2-8)
Instead of disrupting your gut bacteria as Metformin does, we focus on strategic microbiome support:
- Introducing specific prebiotic fibers that feed beneficial bacteria
- Adding targeted probiotic strains including Lactobacillus rhamnosus and Bifidobacterium lactis
- Incorporating polyphenol-rich foods that support microbial diversity
As your microbiome rebalances, you’ll notice:
- Improved digestion (no more bloating or bathroom emergencies)
- Reduced inflammation throughout your body
- Enhanced production of short-chain fatty acids that improve insulin sensitivity
The science: A healthy microbiome produces metabolites that help regulate the expression of genes involved in glucose and lipid metabolism.
A 2019 study in Nature Medicine found that women with PCOS had altered gut microbiota, with decreased microbial diversity and changes in specific bacterial strains (Liu et al., 2019).
https://www.nature.com/articles/s41591-019-0509-0
Step 4: Hormone Support Through Targeted Nutrients (Weeks 4-12)
As insulin levels normalize and inflammation decreases, we provide specific nutrients that support healthy hormone production and metabolism:
- Myo-inositol and D-chiro-inositol 40:1 ratio
- N-acetylcysteine to support glutathione production and androgen metabolism
- Magnesium glycinate for improved insulin signaling and reduced cravings
- Zinc and selenium to support healthy thyroid function (often compromised in PCOS)
The science: Inositols act as second messengers in insulin signaling pathways, effectively mimicking insulin action without side effects.
Clinical trials show they improve ovulation rates comparable to Metformin but with better tolerability and safety profiles. Yet most doctors won’t even mention these alternatives!
Step 5: Lifestyle Integration for Sustained Results (Months 3-6)
While nutrition and supplements create the foundation, sustainable hormone balance requires addressing the lifestyle factors that impact PCOS:
- Strategic movement patterns (like post-meal walking) that improve glucose disposal
- Sleep hygiene practices that stabilize cortisol rhythms
- Stress management techniques that reduce inflammatory cytokines
- Environmental toxin reduction to minimize endocrine-disrupting compounds
The science: Even 10 minutes of movement after meals can improve glucose uptake significantly.
And just one night of poor sleep can reduce insulin sensitivity, showing how critical these factors are for PCOS management.
This is the knowledge about YOUR body they should be teaching!
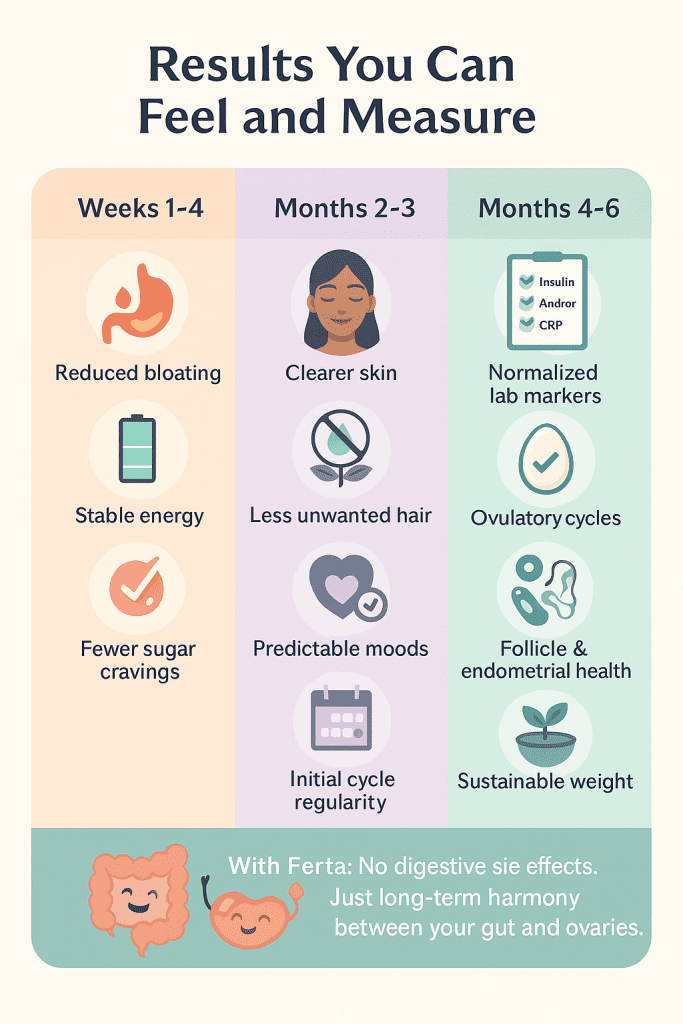
Results You Can Feel and Measure
Unlike the abrupt, uncomfortable changes Metformin creates, the Ferta approach leads to gradual, sustainable improvements:
Weeks 1-4:
- Reduced bloating and digestive discomfort
- More stable energy levels throughout the day
- Fewer carb and sugar cravings
Months 2-3:
- Improved skin clarity
- Reduction in unwanted hair growth
- More predictable moods
- Initial improvements in cycle regularity
Months 4-6:
- Normalized laboratory markers (insulin, androgens, inflammation)
- Regular ovulatory cycles for most women
- Improved fertility markers including follicle development and endometrial thickness
- Sustainable weight management without restrictive dieting
Most importantly, these changes happen without the digestive devastation of Metformin.
Your gut and ovaries can finally be on the same team instead of at war with each other.
The Truth About Your Body’s Healing Power
We built Ferta because we believe women with PCOS deserve comprehensive care, not just symptom management that profits pharmaceutical companies.
Your body has an innate wisdom and healing capacity that the medical system rarely acknowledges.
When given the right support, your hormones can find their natural balance again. Your cycles can regulate.
Your fertility can return. Your metabolism can function optimally.
And you can do it all without planning your life around bathroom access or living with constant digestive distress.
The medical establishment wants you to believe that synthetic drugs are your only option.
That your body is broken and needs pharmaceutical intervention to function properly.
But peer-reviewed research shows that with the right nutrition, supplements, and lifestyle approach, your body can heal itself from PCOS without the side effects.
If you’re tired of the Metformin rollercoaster and ready for a solution that works with your body instead of against it, we’re here to help.
Take our quick fertility quiz to see if our comprehensive PCOS program is right for you.
[Start Your Assessment – Takes Just 2 Minutes]
We’re with you every step of the way.
– The Ferta Team



